A thoughtful and thorough article was recently published about the role and position of artificial intelligence in healthcare with the title Artificial intelligence was supposed to transform health care. It hasn’t on a US website known for its political analyses.
In the USA, in the first half of 2022, 3 billion dollars, while in 2021, 10 billion dollars were directed in the health sector towards startups that also use artificial intelligence, which promised serious potential.
The article examines the reasons why the expectation that the British cognitive psychologist Geoffrey Hinton, one of the “godfathers” of artificial intelligence predicted in 2016 was not fulfilled. Hinton said, that the training of radiologists can be safely stopped since, in 5 years inside, machine learning algorithms will know better than trained doctors what to do. Fortunately, the training of radiologists has not been abolished, and the results of various image scans are still best interpreted by specialists.
We take a look at the difficulties and obstacles along the lines of the three areas highlighted in the writing of Ben Leonard and Ruth Reader.
The fragmentation of the industry
The primary problem is the fragmented healthcare infrastructure, which applies to the whole sector, so it also occurs in the IT area. Communication between systems in different institutions, and even between different departments within the same institution, is not resolved. This affects the treatment of patients as well as the unification and analysis of data and the research and development of various diseases and cures. Artificial intelligence uses available data, but diversified data cannot be unified. Algorithms cannot produce the expected, high-quality conclusions and calculations without the quantity and quality of data essential for machine learning.
In the United States, this is a much more serious problem than in the European (and, of course, Hungarian) healthcare system, which operates with a significant state role. In the USA, the solution is also much more difficult, since the powers of the supervisory bodies are limited, so the institutions, the authorities, and the technology companies must solve this problem together.
The solution is not helped by the fact that, due to technological uncertainties and the fragmented health infrastructure, many institutions have started their development. The local solution may even be ideal, but it actually starts a vicious circle, since the resulting local development, even if it is of a very high standard, necessarily increases the difference between the individual institutions even further.
Uncertainties and gaps in the regulation
There are difficulties in both data management and regulating the applicability of the technology. The use of various personal and sensitive data is often unclear. In Europe, the field is mainly managed by the GDPR, but in America, the regulatory environment is also much more fragmented, there is no framework corresponding to European regulations.
Regulation of the standards and operational frameworks of technology, artificial intelligence, and machine learning is also progressing with difficulty. In the case of which disease groups and symptoms, under what conditions, in what role, with what accuracy, based on what standards, healthcare solutions based on artificial intelligence can be applied?
The American authority, the American Food and Drug Administration (FDA), published its guidelines in this direction only in 2021, and although it has approved more than 300 clinical AI solutions since 1997, it seems that the regulation is only lagging behind the rapidly developing technology. In the United Kingdom, for example, the originally 2014 regulation, which stipulates what kind of software application can be considered a medical device, has been amended twice this year. In Europe, regulation of the applicability of technological solutions can be a problem due to the often different and often conflicting interests and decisions of the member states and national supervisory bodies.
Difficulties in applying the technology
Artificial intelligence has now become indispensable in many areas of healthcare, from an accurate diagnosis to billing. However, many healthcare institutions feel that the technological solutions offered to them do not work properly in the real hospital environment. In theory, everything is very nice, but the adaptation to the local infrastructure runs into significant obstacles, requires significant local resources, and because of this – despite the acceptable basic price of the technological solution – the adaptation to the institution often becomes financially difficult.
Hospital managers also complain that it is not always clear why the algorithm reaches certain results, which is extremely risky in healthcare and can often be measured in human lives.
Despite the outlined difficulties, we are aware of many successful projects, but according to surveys, the health sector is still in second to last place in terms of job opportunities requiring knowledge of artificial intelligence, which indicates that the pace of catching up is much slower than expected. The reason for this is, in addition to the previously mentioned problems, the complexity of the area and the relatively slow pay-off.
Share of Jobs Requiring Knowledge of Artificial Intelligence by Industry in the United States (2020)
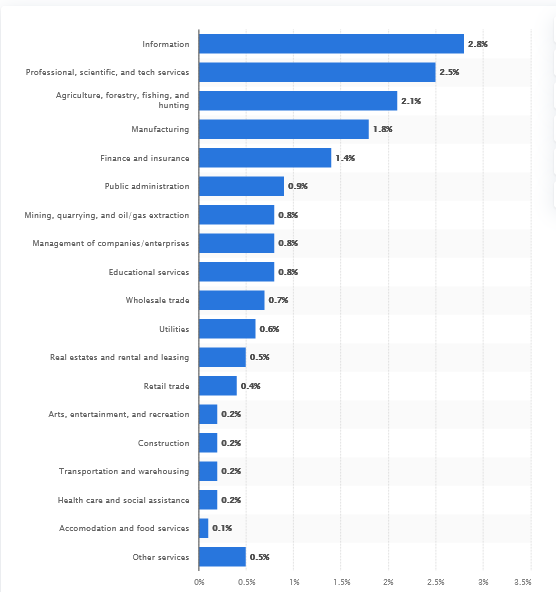
Source: The Burning Glass Institute
Tech companies are also aware of these difficulties, E-Group has faced the industry’s problems up close through the Smart Datalake Platform (DLX) project.
Together with the University of Pécs, we have launched several projects involving health, legal, and IT fields, the technological base of which is the DLX. The flexibility of the ecosystem enables adaptation to the existing infrastructure; therefore, it can contribute to the mitigation of industry fragmentation, and the various data sources enter the data lake in their original unstructured form and can be combined with other existing, structured data.
The DLX also complies with the GDPR, data utilization takes place in the local environment, so sensitive data does not get out of individual closed systems.
Results of already started and planned clinical projects – researches based on real word clinical data, migraine or epilepsy attack prediction, stroke research, etc. – are so far promising and the cooperation with health institutions can also be said to be fruitful, and the various reports expand the possibilities of the application of the results. The most spectacular result of the collaboration is the drug repositioning development, the Repo-x project, the result of which is a patent-pending anti-cancer drug. DLX is an excellent tool for testing institutional and research hypotheses, to which E-Group’s scientific background and existing experience contribute, supplemented by the expertise of our healthcare partners.
Where is the relationship between health tech and artificial intelligence headed? Hinton has now refined his statement. He predicts the breakthrough for 2026 and does not completely rule out radiologists, rather he says that artificial intelligence will be better at interpreting many medical imaging procedures than most specialists. In other words, the human factor remains indispensable. Analysts expect clear results in three areas by 2030. AI powered healthcare systems will predict certain disease risks of patients, offering the appropriate treatment. Access to data will be easier in many areas by applying data lakes and data management platforms, the systems will be connected what will change the physical structure of the institutions, the hospitals will operates in a network, and will be specialized and for many treatments there will be no need for big institutions. With the help of artificial intelligence, patient pathways will be shortened, so patient waiting times will decrease and the efficiency of institutions will increase and also the administrative burden will be reduced.
The future looks bright, but now we know, that the way to it is not as easy as we thought.